The role of platelets in bone marrow aspiration concentrate
PRP and bone marrow aspiration concentrate (BMAC) are being used for a series of clinical treatments in office environment and surgery because of their regenerative benefits in MSK and spinal diseases, chronic pain management and soft tissue indications. PRP not only regulates cell migration and cell proliferation, but also contributes to angiogenesis and ECM remodeling to create a favorable microenvironment and promote tissue repair and regeneration.
BMAC repair process
BMACs are heterogeneous cell compositions containing BMMSCs, making them an endogenous cell source for regenerative medicine repair therapy. They play a role by reducing cell apoptosis, fibrosis and inflammation; And activate the cascade reaction leading to cell proliferation. In addition, BMMSCs have the potential to differentiate into a variety of cell lineages, including osteoblasts, adipocytes, myoblasts, epithelial cells and neurons. They also promote angiogenesis through paracrine and autocrine pathways. It is also important that BMMSC is a contributor to the immune regulation independent of immune specific cells, which participate in the inflammatory stage of wound repair. In addition, BMMSCs support the recruitment of cells to new angiogenesis treatment sites to accelerate local blood flow reconstruction. Jin et al. It was proved that in the absence of sufficient scaffolds, the survival rate of BMMSC and its repair and differentiation ability to promote healing were damaged. Although the tissue collection, specimen preparation and mechanism of action of PRP and BMAC are different, studies show that they can complement each other. In fact, combining PRP and BMAC into a biological product may have additional advantages.
Combining PRP and BMAC
According to some little-known research, the basic principle of combining PRP and BMAC is based on several premises. First, PRP can provide a suitable microenvironment in which BMSC can enhance cell proliferation and differentiation and increase angiogenesis. Secondly, PRP has been used as a scaffold for these cells together with BMAC. On the contrary, the combination of PRP and BMAC can become a powerful biological tool to attract BMMSC population. PRP-BMAC compound has been used to treat tendinosis, wounds, spinal cord injuries, degenerative intervertebral discs and osteochondral defects with great regeneration potential. Unfortunately, although heterogeneous bone marrow cell components include platelets, few reports mention the concentration of platelets in extracted bone marrow and after BMAC treatment, but they can be extracted by appropriate aspiration methods. Further research is needed to understand whether additional platelet concentrates need to be used in combination with BMAC. At present, there is no data on the optimal ratio of platelets to MSC (or other bone marrow cells) cells, which has a positive impact on the nutritional mechanism of MSC in tissue repair. Ideally, bone marrow collection equipment and technology can be optimized to extract enough bone marrow platelets.
PRP growth factor and BMAC nutritional effect
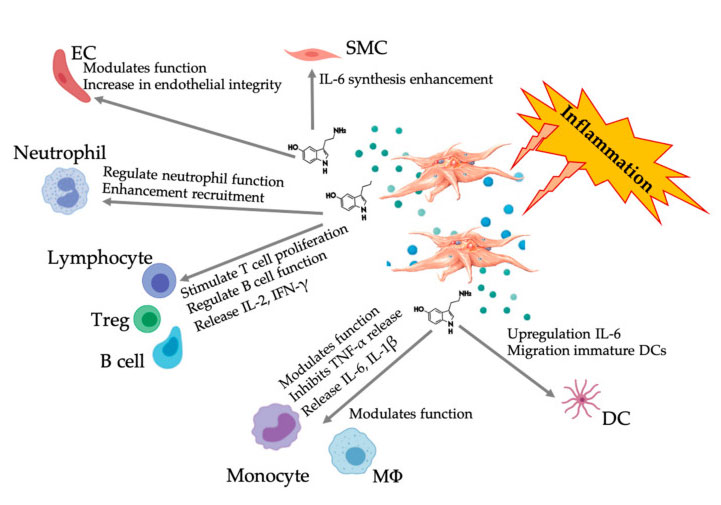
PRP platelet growth factor is a key protein involved in the repair process of BMAC. The diversity of PGF and other cytokines involved in the nutritional process of BMAC can initiate tissue repair by reducing cell apoptosis, anabolism and anti-inflammatory effects, and activating cell proliferation, differentiation and angiogenesis through paracrine and autocrine pathways.
Platelet-derived growth factor and dense granule components are obviously involved in the nutritional process of BMAC and support the tissue repair and regeneration induced by MSC. Abbreviations: MSC: mesenchymal stem cells, HSC: hematopoietic stem cells.
Obviously, in the treatment of OA, PDGF plays a specific role in cartilage regeneration and maintenance of homeostasis through MSC proliferation and inhibition of IL-1-induced chondrocyte apoptosis and inflammation. In addition, three TGF- β The subtypes are active in stimulating cartilage formation and inhibiting inflammation, and they show the ability to promote MSC-related tissue healing through intermolecular interaction. The nutritional effect of MSC is related to the activity of PGF and the secretion of repair cytokines. Ideally, all these cytokines should be present in the BMAC treatment bottle and transported to the tissue injury site to promote the best MSC-related therapeutic tissue healing.
In a joint OA study, Mui ñ os-L ó pez et al. It shows that MSC derived from synovial tissue has changed function, resulting in the loss of its recovery ability. Interestingly, the direct injection of PRP into the subchondral bone of osteoarthritis resulted in the reduction of MSC in synovial fluid, indicating clinical improvement. The therapeutic effect is mediated by reducing the inflammatory process in the synovial fluid of OA patients.
There is little information available about the presence or concentration of PGF in BMAC or the ideal ratio required to support the nutritional function of BMMSC. Some clinicians combine high PRP concentration with BMAC to obtain more biologically active grafts, which is expected to optimize the treatment results of regenerative medicine. However, there are few available safety and efficacy data, indicating that combining high PRP concentration with BMAC is a more effective treatment option. Therefore, we believe that it may not be appropriate to manipulate BMMSC by activating them with high platelet concentration at this stage.
Interaction of platelets with antiplatelet drugs and NSAIDs
PRP contains a broad spectrum of secretory components and is composed of many biological media. The therapeutic effect of PRP is attributed to these mediators. Although the therapeutic mediators in platelets are well known, the optimal formulation and kinetics of these anabolic and catabolic drugs are not completely clear. One of the main limitations of achieving therapeutic formulations is to overcome the variability of these biological mediators in order to target the well-regulated downstream effects that are always repeatable and clinically beneficial. For this reason, drugs (such as non-steroidal anti-inflammatory drugs (NSAIDs)) can affect the release of platelet secretory groups. In a recent open-label fixed-sequence study, daily intake of 81 mg of aspirin (ASA) reduced the expression of key mediators, such as TGF- β 1. PDGF and VEGF.
These effects are attributed to the irreversible inhibition of cyclooxygenase-1 (COX-1) and the adjustable inhibition of cyclooxygenase-2 (COX-2), which are two enzymes required for downstream platelet degranulation. A recent systematic review found that antiplatelet drugs may reduce the growth factor release curve in a COX-1 and COX-2 dependent manner, and 8 of the 15 studies found that growth factors decreased.
Drugs (e.g. NSAIDs) are usually used to relieve pain and reduce inflammation caused by MSK disease. The mechanism of NSAIDs is to inhibit platelet activation by irreversibly binding with COX enzyme and regulating arachidonic acid pathway. Therefore, the function of platelets will change during the whole life cycle of platelets, thus preventing PGF signal transmission. NSAIDs inhibit cytokine production (e.g., PDGF, FGF, VEGF, and IL-1 β, IL-6, and IL-8), while enhancing TNF- α。 However, there is little data on the molecular impact of NSAIDs on PRP. There is no consensus on the best time for the preparation and administration of PRP in patients who use NSAIDs. Mannava and colleagues quantified the anabolic and catabolic biological factors in the leucocyte-rich PRP of healthy volunteers taking naproxen. They found that after using naproxen for one week, the levels of PDGF-AA and PDGF-AB (effective mitogen for promoting angiogenesis) were significantly reduced. After one week, the level of growth factor returned to near the baseline level. After using naproxen for one week, the LR-PRP level of proinflammatory and catabolic factor IL-6 also decreased, and returned to the baseline level after a one-week clearance period. At present, there is no clinical study to prove that patients with naproxen after PRP treatment have negative results; However, it is recommended to consider a one-week washing period to restore the PDGF-AA, PDGF-BB and IL-6 values to the baseline level to improve their biological activity. More research is needed to fully understand the effects of antiplatelet and NSAID on PRP secretion group and its downstream targets.
Combine the application of platelet-rich plasma with rehabilitation
Although basic scientific research shows that physical therapy and mechanical load have a clear role in the recovery of tendon structure after PRP injection, there is no consensus on the best rehabilitation plan for MSK disease after PRP treatment.
PRP treatment includes injection of concentrated platelets in local tissue environment to regulate pain and promote tissue repair. The strongest clinical evidence exists in knee OA. However, the use of PRP in the treatment of symptomatic tendinosis is controversial, and the reported results are different. Animal studies usually show histological improvement of tendinosis after PRP infiltration. These studies show that mechanical load can regenerate tendons, and the load and PRP injection work together to promote tendon healing. Differences in PRP preparations, biological preparations, preparations, injection schemes and tendon injury subtypes may lead to differences in clinical results. In addition, although scientific evidence supports the benefits of rehabilitation plans, few published clinical investigations attempt to manage and integrate consistent post-PRP rehabilitation plans.
Recently, Onishi et al. The role of mechanical load and PRP biological effect in Achilles tendon disease was reviewed. They evaluated the phase I and phase II clinical studies of Achilles tendon disease treated with PRP, focusing on the rehabilitation plan after PRP injection. Supervised rehabilitation programs seem to improve exercise compliance and improve results and the ability to monitor exercise dose. Several well-designed Achilles tendon PRP trials combined post-PRP treatment with mechanical load rehabilitation plan as an integral part of the regeneration strategy.
Future outlook and conclusions
The technical progress of PRP equipment and preparation methods shows promising patient results, although the definition of different PRP biological agents and the relevant biological characteristics of the final product are still inconclusive. In addition, the full potential of PRP indications and applications has not been determined. Until recently, PRP has been commercially sold as an autologous blood derivative product, which may provide doctors with the ability to use autologous platelet growth factor technology in specific indicated pathology and diseases. At first, the only criterion for successful application of PRP that is often cited is the prepared sample, whose platelet concentration is higher than the whole blood value. Today, fortunately, practitioners have a more comprehensive understanding of the operation of PRP.
In this review, we acknowledge that there is still a lack of standardization and classification in the preparation technology; Therefore, there is no consensus on PRP biological agents at present, although more literature has reached agreement on the effective platelet dose concentration required to promote (new) angiogenesis. Here, we briefly introduced the activity of PGFs, but more broadly reflected the specific platelet mechanism and effector effect of white blood cells and MSCs, as well as the subsequent cell-cell interaction. In particular, the presence of white blood cells in PRP preparations provides a deeper understanding of harmful or beneficial effects. The clear role of platelets and their interaction with innate and adaptive immune systems have been discussed. In addition, sufficient and well-documented clinical studies are needed to determine the full potential and therapeutic effect of PRP in various indications.
(The contents of this article are reprinted, and we do not provide any express or implied guarantee for the accuracy, reliability or completeness of the contents contained in this article, and are not responsible for the opinions of this article, please understand.)
Post time: Mar-01-2023